Svært mye interessant i denne studien om pusten og CO2. Spesielt avsnittene om at kronisk smerte endrer pustemønsteret og senker CO2 nivået i kroppen.
http://www.ncbi.nlm.nih.gov/pubmed/11530714
http://www.mental-mechanics.org/pdf/Anxiety/FH%20Wilhelm%20et%20al%20-%20Respiratory%20dysregulation%20review.pdf
CHRONIC PAIN
Acute pain results in shortness of breath and an increase in ventila- tion (Nishino, Shimoyama, Ide, & Isono, 1999). A commonly used pain provocation in the laboratory is immersion of a limb into almost freezing water (cold pressor test), which is reliably followed by reduc- tions of PetCO2 among healthy people. (On the other hand, partial or full immersion of the face in cold water causes a modest reduction in ventilation, a component of the diving response). Patients who experi- ence intense chronic pain show these respiratory-related changes over extended periods. For example, migraine headache patients were found to have significantly lowered PetCO2 levels during an attack compared to controls and to migraine-free periods (Hannerz & Jogestrand, 1995), and there were even respiratory abnormalities immediately before an attack (Zhao, Sand, & Sjaastad, 1992). Glynn, Lloyd, & Folkhard (1981) examined arterial pH and PCO2 in 52 chronic pain patients (e.g., back pain, cancer-related pain). PCO2 was mark- edly lowered in these patients, and nerve blockade of pain resulted in a significant rise in PCO2.
Interestingly, blood pH was normal, indicat- ing a long-term blood chemistry compensation for chronic hyperven- tilation. In a sleep study of fibromyalgia patients, a high incidence of respiratory abnormalities such as periodic breathing were found, and arterial PCO2 was lowered in a subgroup of patients (Sergi et al., 1999). Many clinicians, including one of the present authors (Gevirtz), have had the opportunity to measure PetCO2 levels in hun- dreds of chronic muscle pain patients, and the clinical impression is that these levels are almost universally low (c.f., Timmons & Ley, 1994). Of course, pain may also play a role in the increased ventilation found in the FCD patients discussed above, especially during acute episodes of chest pain.
The increased ventilation during acute pain is likely a component of the fight-flight response, preparing the individual for immediate action and sometimes for being attacked or maybe injured. Interest- ingly, recent evidence from animal studies indicates that acute hyperventilation has anesthetic effects via the adrenergic and endogenous opiate system (Ide et al., 1994a, 1994b). Thus, the increased ventila- tion that first served to activate an individual for a fight may have the beneficial side effect of relieving pain if the fight is lost.
So far, no study we know of has examined if the chronic hyperventi- lation exhibited by pain patients is of any benefit to their pain experi- ence (and thus a coping strategy), is only a side effect of the intense pain, or makes their pain worse. One would expect that chronic hyper- ventilation is not healthy in these patients, as it is in other clinical groups, because it interferes with blood homeostatic mechanisms and can lead to a variety of physical symptoms. It has been suggested that by numbing pain, hyperventilation may become a short-term adaptive process with long-term negative consequences (Conway, 1994). Inter- esting in this context is that opioids are frequently prescribed to chronic pain patients to suppress their pain, and they typically also suppress ventilation via central nervous pathways, sometimes to a lethal extent. In summary, there is some initial evidence that hyper- ventilation plays a role in chronic pain, and some mediating mecha- nisms have been identified. However, most of the pain-hypocapnia relationship in chronic pain syndromes is not well understood.
Chronic Pain
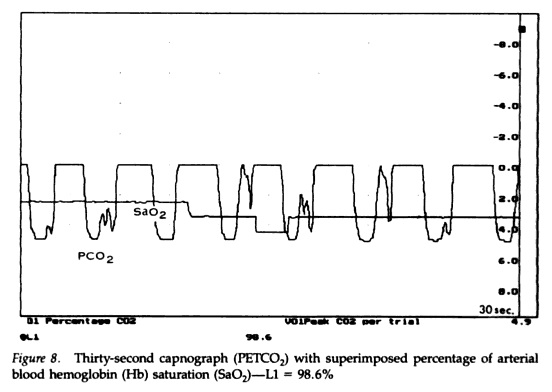
Slow abdominal breathing is often taught as a relaxation technique in preparation for acute pain, such as surgery or childbirth, and it also helps patients counteract their tendency to hyperventilate during such events. As described above, the chronic hyperventilation that can accompany long-lasting pain may be especially problematic because it may have long-term negative organismic effects. It is therefore logi- cal that breathing training could be a valuable asset in the overall treat- ment of chronic pain disorders. However, no data are currently avail- able on the role of breathing training as a systematic intervention in these disorders. It is one author’s (Gevirtz) clinical experience that breathing training is in fact a powerful tool in a comprehensive pain management protocol. This is also a common assumption of most bodywork therapies of pain (c.f., Clifton-Smith, 1998). Here again, the capnometry readings are used to illustrate the physiological basis of the symptomatology.
Muscular pain can result from chronically tense muscles. Hubbard, Gevirtz, and their colleagues recently showed that a sympathetically mediated pathway to muscle spindles (trigger points), rather than pathways to muscle fibers, plays an important role in the maintenance of chronic muscular pain (Gerwin, Shannon, Hong, Hubbard, & Gevirtz, 1997; Hubbard & Berkoff, 1993; McNulty, Gevirtz, Hub- bard, & Berkoff, 1994). Psychological stress increased the activity of these spindles, which suggests that stress reduction could alleviate chronic muscle pain. Thus, relaxation induced by slow diaphragmatic breathing may have a beneficial effect on the activation of these spin- dles and reduce general muscle tension.