Veldig spennende studie som nevner at HRV trening av pusten har langtids virkninger på hjerte/kar sykdommer og at det aktiverer nevroplastisitet, altså vari endring i nervesystemet. Bekrefter at pustefrekvensen på 6x /min (5 sek inn, 5 sek ut), gir en opptrening vagusnerven. Viser også at man får effekt uten biofeedback, men nervesystemet resonderer bedre med biofeedback.
http://www.ncbi.nlm.nih.gov/pubmed/14508023
http://www.psychosomaticmedicine.org/content/65/5/796.long
http://journals.lww.com/psychosomaticmedicine/Fulltext/2003/09000/Heart_Rate_Variability_Biofeedback_Increases.12.aspx
Abstract
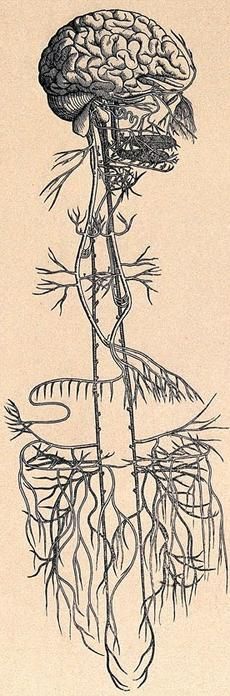
OBJECTIVE: We evaluated heart rate variability biofeedback as a method for increasing vagal baroreflex gain and improving pulmonary function among 54 healthy adults.
METHODS: We compared 10 sessions of biofeedback training with an uninstructed control. Cognitive and physiological effects were measured in four of the sessions.
RESULTS: We found acute increases in low-frequency and total spectrum heart rate variability, and in vagal baroreflex gain, correlated with slow breathing during biofeedback periods. Increased baseline baroreflex gain also occurred across sessions in the biofeedback group, independent of respiratory changes, and peak expiratory flow increased in this group, independently of cardiovascular changes. Biofeedback was accompanied by fewer adverse relaxation side effects than the control condition.
CONCLUSIONS: Heart rate variability biofeedback had strong long-term influences on resting baroreflex gain and pulmonary function. It should be examined as a method for treating cardiovascular and pulmonary diseases. Also, this study demonstrates neuroplasticity of the baroreflex.
The resonant HRV frequency usually is ∼0.1 Hz (6 cycles/min). At this frequency, we previously found that HR and BP oscillate 180° out of phase (20), while HR and respiration oscillate in phase with each other (0° phase relationship, with inhalation coinciding with HR accelerations and exhalation with decelerations). Thus, when people breathe at their resonant frequency, respiratory effects on HRV stimulate baroreflex effects (ie, as the individual inhales, HR rises, BP falls, and the consequent baroreflex response produces a further increase in HR, with corresponding effects during exhalation). The consequent resonance effects produce very large increases in both HRV and baroreflex gain, which can be obtained only when subjects try to increase HRV at this particular frequency (20).

Biofeedback acutely increased both HRV and baroreflex gain, and chronically increased baroreflex gain and peak expiratory flow even among healthy individuals, in whom these measures ordinarily are thought to be stable. Other interventions known to increase baroreflex gain, including β-adrenergic blockade (30) and exercise training (31), also prevent sudden death in high-risk populations. Further research may show that HRV biofeedback training may have similar salutary effects, without the side effects that medication often causes.
The acute baroreflex effects are consistent with our hypothesis that stimulation of HRV at its resonant frequency by respiratory activity involves amplification of the vagal baroreflex response, and that this “exercises” the baroreflex.
However, the cumulative changes in baroreflex gain, both within and, more importantly, across sessions, were not simple effects of slow breathing. The effects of biofeedback on baroreflex gain, both within and between sessions, remained significant, after factoring out the effects of respiration rate. Thus, although breathing at participants’ resonant frequencies produced immediate baroreflex augmentation, over time (both within individual sessions and over weeks of practice) the baroreflex became intrinsically more responsive, an effect that no longer depended on breathing rate and volume. Thus, the intrinsic resting baroreflex increased.