Nevner hvordan pusten har sammenheng med smerter, spesielt i nakke, og beskriver normal vs abnormal pustefunksjon.
http://reactivemovement.com/images/stories/pain%20and%20faulty%20breathing.pdf
http://www.bodyworkmovementtherapies.com/article/S1360-8592(03)00085-8/abstract
«Breathing mechanics are influenced directly by
- * Bio-mechanical factors such as rib head fixations or classical upper/lower crossed patterns of muscle imbalance.
- * Biochemical factors involving anything that affects the body’s delicate pH balance including allergy, infection, poor diet, hormonal influences or kidney dysfunction.
- * Psychosocial factors such as chronic anxiety, anger or depression. «
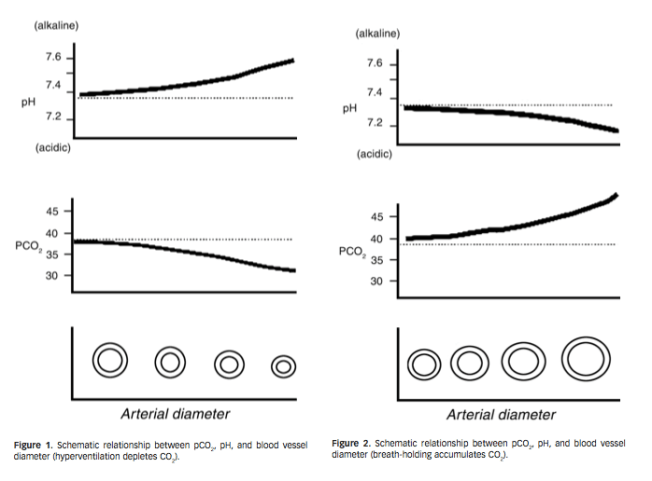
«For example, ketoacidosis, a byproduct of a very popular diet which promotes high protein/low carbohydrate intake, increases the acidic state of the blood which will promote deeper, faster breathing (the higher CO2 content stimulates the breathing drive).»
«Alkalosis causes a decrease in the threshold of peripheral nerve firing, an increase in muscular tension, muscle spasm, spinal reflexes and significantly heightened perception of pain, light and sound. Alkalosis can also result in emotional lability and produce a sense of apprehension and anxiety that frequently leads to panic attacks and phobic behavior (Chaitow et al., 2002; Chaitow, 2000).»
«With each normal (resting) breath this bucket handle movement occurs at every rib level, which has a gentle micro-massaging effect maintaining healthy spinal movement, blood and nutritional flow to the musculo-skeletal struc- tures.»

«Although the pectoralis major, pectoralis minor, latissimus dorsi, serratus anterior and trapezius are not typically considered accessory respiratory muscles, they assume a more respiratory than postural function in the dysfunctional or paradoxical breath- er and contribute to the faulty pattern of lifting the ribcage up during inspiration (Hruska, 1997). When chest lifting becomes a faulty breathing pattern, chronic lifting of the clavicles creates the appearance of deep clavicular grooves as seen in Fig. 5 (Lewit, 1999).»

«The same criteria were applied for normal (relaxed) breathing as for deep breathing. A ‘‘normal’’ breath according to these criteria would:
- Initiate in the abdomen, which would expand outward during inhalation and inward during exhalation.
- Have some degree of horizontal lower rib motion (even if slight).
- Have no lifting up motion in the upper ribs.
- Have no clavicular grooves. «
«Only one type of pain had a statistically significant relationship with faulty breathing – neck pain»
«This study showed that 87.2% of the participants have experienced some sort of musculo-skeletal pain. This high percentage is no surprise. What was remarkable were the high percentages of this sample population with faulty breathing me- chanics; 56.4% of the population studied had faulty relaxed breathing and 75% showed faulty breathing when taking a deep breath. »
«If the results of this study reflect the general population, as clinicians your chances are 3 in 4 that the new patient you see today will have some level of abnormal breathing patterns.»
«But why is the relationship between faulty breathing and neck pain so pervasive?
The answer may be simply that the most common fault in respiration of lifting the thorax with the accessory muscles of respiration instead of widen- ing it in the horizontal plane overstrains the cervical spine and musculature, contributing to recurrent cervical syndromes (Lewit, 1999)»
«He especially found this in patients with forward head postures, temporo-mandibular dysfunction and chronic sinus problems. Clinically, Hruska has identified hemidiaphragm hypertonicity complementing ipsilateral abdominal and oblique muscle weakness and contra lateral cervical symptoms (Hruska, 1997).»
«This study has shown that normal patterns of breathing are the exception rather than the rule. An overwhelming 75% of those studied exhibited faulty breathing mechanics. If the results of this study reflect the general population, as clinicians, your chances are 3 in 4 that the new patient you see today will have faulty breath- ing patterns.»