Nevner hvordan smerteopplevelse blir mindre med meditasjon, men viser også til at det sannsynligvis er pustefrekvensen som gir den smertestillende effekten. Pluss den nevner hvordan frontallappen bidrar med smertestillende opioider.
http://www.psychosomaticmedicine.org/content/71/1/106.long
These results indicated that Zen meditators have lower pain sensitivity and experience analgesic effects during mindful states. Results may reflect cognitive/self-regulatory skills related to the concept of mindfulness and/or altered respiratory patterns.
Mindfulness can be described as an equanimous state of observation of one’s own immediate and ongoing experience.
Mindfulness has been described as “intentional self-regulation of attention from moment to moment … of a constantly changing field of objects … to include, ultimately, all physical and mental events….” (5). Furthermore, an attitude of acceptance toward any and all experience is stressed. Traditional accounts of mental and emotional transformation accompanying mindful practice (6,7) are supported by scientific findings of psychological and biological effects on practitioners (8–10) and patients (5,11–15).
Mindfulness-based therapies have reported success treating anxiety (11,15), obsessive compulsive disorder (13), and depression (12,14). Positive correlations between meditation experience of Buddhist monks and positive affect (10) have been reported. Increases in positive affect have also been observed in a longitudinal study in which naïve subjects were trained to meditate (8).
It is well known that cognitive manipulations, such as hypnosis, attention, expectancy or placebo, can influence the experience of pain and the associated neurophysiological activity (17–19). There is also mounting evidence that mindfulness may be effective in treating chronic pain.
Significant positive improvements were found on all measures immediately after the 10-week training program. However, follow-up evaluation showed stable improvements on most measures with the exception of present moment pain. The authors interpreted the results as the acquisition of an effective coping strategy for pain, where the pain itself did not change but the relation or stance taken toward the pain was positively altered.

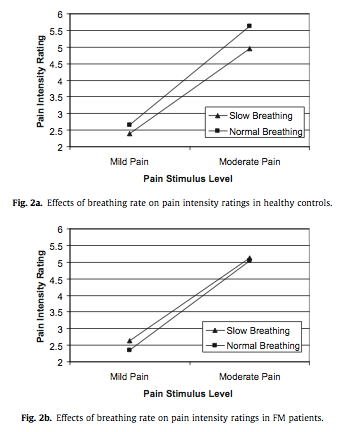
Changes in pain were further examined in relationship to meditation training. The amount of meditation experience of individual practitioners predicted the degree of pain intensity modulation (i.e., versus baseline) with more hours of experience leading to greater reductions in pain intensity during the mindfulness condition [r(9) = −.82, p< .01].

Notably, pain modulation induced by mindfulness (relative to baseline-1) was correlated with the corresponding changes in respiratory rate across all subjects [intensity: r(23) = .37, p = .03; unpleasantness: r(23) = .42, p = .02]. Furthermore, the significant decrease in pain intensity reported above in the meditators during the mindfulness condition relative to baseline-1 (Figure 2) did not reach significance after including the changes in respiration as a covariate [F(1,11) = 3.02, p = .11]. In contrast, the significant increase in pain intensity reported by the control subjects in the concentration condition remained significant after accounting for changes in respiratory rates [F(1,11) = 20.94, p = .001]. These effects suggest that the changes in pain induced by mindfulness, but not concentration, may be at least partly accounted for by changes in respiration.
The main findings are the following:
- 1) Meditators required hotter temperatures than controls to experience moderate pain.
- 2) As hypothesized, meditators experienced less pain while attending mindfully, whereas control subjects did not show such modulation.
- 3) Unexpectedly, analgesic effects of mindfulness were more clear on the sensory dimension of pain (i.e., perceived intensity) than the affective dimension of pain (i.e., pain unpleasantness), although effects were observed in the same direction.
- 4) The magnitude of the analgesic effect of mindfulness was predicted by the number of hours of meditation practice in meditators.
- 5) When attention was directed toward the stimulation, with no mention of attending mindfully, control subjects showed the expected increase in pain intensity and unpleasantness whereas meditators did not differ from baseline.
- 6) Physiologically, meditators had slower breathing rates than controls, consistent with their self-assessed reduced reactivity. Importantly, changes in respiratory rate predicted the changes in felt pain and the analgesic effect of mindfulness states was no longer significant after accounting for changes in respiratory rates (covariance).
- 7) On a mindfulness scale, meditators scored higher on the tendency to be observant and nonreactive. Higher scores on these dimensions of mindfulness were further associated with lower pain sensitivity and slower respiratory rates.
Zen meditation was associated with lower pain sensitivity as demonstrated by the higher temperatures required to produce moderate pain. The observed difference (49.9°C versus 48.2°C) should be considered large as it typically corresponds to an increase of about 50% on a ratio scale of pain perception or 20 to 25 points on a 0 to 100 numerical pain scale, based on similar psychophysical methods (28,33).
While attending mindfully, the Zen practitioners showed reductions of 18% pain intensity. Remarkably, individuals with more extensive training experienced greater reduction in pain. This finding is extremely important as it suggests that the observed pain reduction may not simply reflect a predisposition to meditation (individual differences) but may also involve experience-dependent changes associated with practice. This is in line with other studies linking meditation training with mindfulness, medical symptoms, and well-being (16); attention performance, anxiety, depression, anger, cortisol and immunoreactivity (34); an inverted U-shaped function of attention-related brain activity (35); electrophysiological markers of positive affect (10); positive affect and stronger immune responses (8); and cortical thickness and gray matter density (9,36,37).
The analgesic effects of mindful attention may relate to the physiological state induced as suggested by the respiration data. Overall, the meditators breathed at a slower rate than control subjects in all conditions and their mean respiratory pattern followed that of their pain ratings. In contrast, respiratory rate did not change noticeably across conditions in the control subjects. Slower breathing rates (typically meditators) were associated with less reactivity and with lower pain sensitivity. These relationships suggested that the meditators were in a more relaxed, nonreactive physiological state throughout the study, which culminated in the mindfulness condition and which influenced the degree to which they experienced pain.
The covariance analysis suggested that this analgesic effect could be mediated at least in part by the observed change in respiration.
A neuro-chemical model of meditation put forth by Newberg and Iversen (47) offers a possible explanation for our results. Meditation practice, involving volitional regulation of attention, seems to activate prefrontal cortex (35,48,49); this has been observed during Zen practice (50). Increases in prefrontal activation can stimulate the production of b-endorphin (e.g., in the arcuate nucleus of the hypothalamus) (47). B-endorphin is an opiate associated with both analgesia and a reduction in respiratory rate as well as decreases in fear and increases in joy and euphoria (47). Interestingly, the direction of attention toward breathing and the volitional control of breathing rates are part of many meditative techniques; however, causation can obviously not be inferred from those observations.
Another related possibility is that meditation leads to reductions in stress and stress-related chemicals, such as cortisol which interact with the opiate system. A reduction of cortisol can greatly enhance the binding potential/efficacy of endogenous opioids (27), possibly contributing to a downregulation of nociceptive responses. Studies have reported evidence of reduced cortisol responses in meditators (34,52,53).